Insight
Tegria’s Biggest Event Takeaways From 2025
2025 was another dynamic year in healthcare, and Tegria took part in the industry’s important conversations. After all we learned in 2024, we knew that this year would bring new momentum, intensified pressures, and evolving priorities across providers and payers alike. In case you couldn’t attend every conference, forum, or exhibition, this post gathers our experts’ event takeaways from the front lines of healthcare at events such as HIMSS25, ViVE 2025, KLAS Patient Consumer & Innovation Summit, and more.
From rapid shifts in outpatient care models and the rise of generative AI across patient access to mounting financial constraints, our team captured not only what leaders are talking about today, but where the industry is headed. Dive in to explore the themes that will shape your strategy, your operations, and your roadmap for the year ahead.
ViVE 2025
This year’s ViVE conference raised an important question: Are we addressing healthcare’s fundamental misalignments or reinforcing them with AI? Tye Cook emphasized the importance of rethinking your operating model before introducing AI. Leaders who implement AI without first aligning their operations risk automating inefficiencies and even creating new challenges. While technology can boost efficiency and expand access, without proper alignment, even the most advanced tools will fall short of their potential.
HIMSS25
At HIMSS25, Tegria shared key findings from The Health Management Academy regarding patient access and experience. The session highlighted the importance of a streamlined, operations-forward approach to technology to achieve improvements in patient access. We also presented with St. Luke’s University Health Network, sharing our journey in building a cloud-based Azure data lakehouse. Another highlight was our Lunch and Learn, where attendees gained practical guidance on how to evaluate AI opportunities. Overall, there were a lot of great sessions on data and information, health equity, technology, governance, and public policy.
MUSE Inspire
Key themes from MUSE Inspire 2025 included AI, interoperability, population health and analytics, cybersecurity, and patient engagement. In addition to those themes, we had the opportunity to share about regulatory compliance and financial performance. We joined Ashley Hall from White River Health to present a collaborative approach to regulatory readiness. Later, we presented an outcomes-focused productivity approach that healthcare organizations can adopt to drive strategic decisions and long-term revenue cycle improvements.
HFMA Annual Conference
The conference centered on three main themes: driving financial and operational transformation, embracing innovation, and prioritizing people. It highlighted how leaders are looking for performance improvement strategies with measurable ROI. Static reports are no longer enough. Leaders want modern data visualization tools to help them focus on the right priorities and act quickly. AI also generated strong interest at the conference. However, with limited resources, leaders are cautious and expecting proven ROI before committing. Denials were also top of mind, with a strong interest in technologies that can help ease the burden on staff and improve results.
AHA Leadership Summit
The AHA Leadership Summit reinforced a central truth about what matters most in healthcare transformation: people. Key themes included partnership, investing in the employee experience, effective change management, patient access, and people-first transformation.
At the summit we heard, “People don’t resist change—they resist uncertainty.” Leaders who intentionally embed change management into every initiative can better equip their teams to thrive. While technology plays an important role, we find lasting impact comes from cultivating a strong culture, building trust, and leading with compassion.
KLAS Patient & Consumer Innovation Summit
A key message from the summit was that meaningful innovation starts with listening to patients and designing around their needs. Today, organizations are intentionally incorporating patient feedback into strategic decisions, which improves patient satisfaction, trust, and loyalty. AI, when used well, can support more personalized, understandable interactions. The summit also emphasized offering patient education in multiple, on-demand formats to empower patients to make more informed decisions. Insights from the KLAS Patient & Consumer Innovation Summit reflect a broader movement toward patient-centered digital transformation.
MEDITECH LIVE 25
MEDITECH LIVE 25 was MEDITECH’s highest-attended leadership summit to date. A major theme of the event was that modernization is no longer optional. Some vendors are winding down support for legacy platforms, so health systems cannot afford to stand still. Another theme was that AI is moving from concept to embedded strategy. Many sessions showcased how AI solutions embedded within Expanse are driving results. Upgrading to Expanse 2.2 further enables organizations to adopt the latest interoperability features and automation. Lastly, community and collaboration continue to drive progress. MEDITECH LIVE provided an opportunity for providers, technology partners, and service organizations to come together and reimagine care delivery.
HPA Fall Leadership Forum
From navigating regulatory changes to market pressures and trends, health plan leaders discussed a variety of pressing topics and challenges at the HPA Fall Leadership Forum. During our fireside chat with the Community Health Plan of Washington and Network Health, we discussed payer-provider collaboration, tools for sharing clinical data, and different Epic solutions. While payers are at varying stages of adoption, attendees found it valuable to learn how peers are navigating choices and balancing demands. All in all, the event provided a dynamic space for health plan leaders to engage in meaningful conversations and explore future-focused strategies.
CHIME25 Fall Forum
As we saw at other industry events, AI is increasingly being integrated into everyday operations. IT governance is becoming essential for safe AI deployment, data quality, and strategic alignment. It comes as no surprise that community and rural health systems continue to struggle to keep pace with modernization because of financial strain and overstretched IT teams. CHIME25 highlighted that, while organizations are progressing at different speeds, they face common challenges. Clear governance, practical AI strategies, strong security, and modernization are vital to success.
Thank you for following along with our 2025 event takeaways. We look forward to connecting with you as we continue advancing meaningful conversations in 2026.
Insight
Key Takeaways From CHIME25 Fall Forum
CHIME25 Fall Forum in San Antonio reinforced why this gathering remains one of healthcare’s most valuable spaces for honest conversation and peer learning. Tegria’s attendees, which included Jeff Webber, Managing Director of Enterprise Systems & Services, and Chad Skidmore, VP of Technology Services, spent the week immersed in discussions about modernization, governance, AI, and the realities facing health systems of all sizes.

Here are the themes that stood out.
AI Moving Into Everyday Operations
AI dominated the conference, but the discussions centered on real-world adoption rather than abstract possibilities. Health systems shared examples of ambient clinical tools now in routine use and highlighted fast-growing interest in operational AI aligned with financial and workforce challenges.
AI has very rapidly moved from hype to a range of practical and successful use cases. Ambient technology is already becoming common, and I heard several examples of AI supporting operations in both provider and payer environments.
CHAD SKIDMORE
Organizations are at very different stages, with some implementing AI at scale while others are piloting. Many are still drafting governance and policy frameworks. Community and rural organizations are generally adopting AI through features embedded within existing platforms, especially major EHRs, allowing progress within limited staffing and budgets.
The Growing Importance of Governance
IT governance surfaced as a central theme across multiple sessions. Leaders described an expanding set of responsibilities, with technology decisions now intertwined with financial planning, workforce strategy, clinical operations, and risk mitigation.
IT’s role in organizational governance continues to grow, extending far beyond traditional technology decisions. More leaders are being pulled into broader strategic planning because technology now shapes so much of the organization.
JEFF WEBBER
AI is accelerating this shift. Many organizations are building governance frameworks to ensure safe deployment, manage data quality, track outcomes, and align initiatives with enterprise strategy.
Cybersecurity: Progress With Ongoing Pressure
Cybersecurity remained a top concern. Leaders discussed the lasting impact of recent high-profile attacks, the rise in cyber insurance requirements, and the growing complexity of proposed regulations.
Chad noted that past fear-driven spending pulled resources away from modernization efforts and may increase again as standards tighten. Jeff observed that some of the most mature cybersecurity programs are now led by outside CSOs, often former banking and government security leaders who can bring rigorous practices into healthcare.
Community and Rural Health Struggling To Keep Pace
Sessions focused on community and rural health highlighted widening disparities in digital maturity. Financial strain limits modernization. IT teams are small and often stretched thin. Innovation is slowed not by lack of commitment, but by lack of time, resources, and exposure to peer best practices.
Community health organizations continue to struggle with financial pressures that affect every part of their operations. The result is a widening divide between community organizations and larger urban peers, especially when it comes to innovation and modernization.
CHAD SKIDMORE
People and Relationships Still Define CHIME
Despite the focus on complex technology, the most consistent theme was the power of personal connection. The Forum’s intimate environment encouraged honest dialogue, strong peer interaction, and meaningful relationship-building. The experience reinforced how meaningful it is for healthcare leaders to invest in long-term relationships, returning to shared spaces like CHIME to build trust, exchange ideas, and accelerate progress together.
Looking Ahead
CHIME25 made clear that while organizations are progressing at very different speeds, they share common challenges. Clear governance, practical AI strategies, sustainable security, and a renewed focus on equitable modernization are essential.
Looking to a new season and year, we’re reminded that progress in healthcare technology depends on people. Thoughtful leaders. Collaborative peers. Partners who listen and build solutions grounded in real-world experience. As the industry continues to navigate rapid change, CHIME’s annual forum remains a place where leaders can align on what matters most and move forward with renewed clarity and purpose.
Insight
Driving Sustainable Change in Healthcare: A Conversation With Tegria and KLAS Research
In a recent episode of the “AHA Associates Bringing Value Podcast,” the American Hospital Association sat down with Meg Johnson, director of Care Operations at Tegria, and Robbie Bullough, senior director of consulting at KLAS Research, to discuss why structured change management is a strategic imperative in healthcare transformation. Their conversation explored how healthcare leaders can move beyond implementation checklists to foster true adoption, build trust, and sustain results over time.

Below are key insights from the discussion.
Q: Why is it critical to build change management into transformation strategies from day one?
Meg Johnson:
If you had the chance to make transformation successful, wouldn’t you take it? Research shows that effective change management makes it seven times more likely you’ll achieve your intended outcomes and ROI. Too often, we start with a project plan but forget the change plan—the equivalent groundwork that prepares people to engage and sustain transformation. Without it, organizations risk delays, budget overruns, and even long-term “change fatigue.” You don’t get many chances at large-scale transformation, so it’s vital to start strong.
Robbie Bullough:
When change isn’t planned from the start, costs multiply later—extra training, rework, system redundancies, even staff turnover from burnout. These are invisible costs at first, but very real when they hit. Like maintaining your home appliances, the ROI of doing change management right is that things keep working smoothly.
Q: Who needs to be involved early on to make transformation successful?
Meg Johnson:
Transformation affects everyone differently, so success depends on alignment across all stakeholder groups. Executive sponsors are essential. They must stay visible and engaged throughout the process. But frontline and mid-level leaders also play a critical role. They help uncover resistance early and build support among staff. The most successful organizations bring diverse voices to the table, even from outside their immediate structure, to build broad coalitions of support.
Robbie Bullough:
Operations leaders must have a voice in design and decision-making. When people feel change is done with them instead of to them, adoption rates soar. If operations are left out, resistance builds, and you end up fixing problems that could have been prevented by including them from the beginning.
Q: How can organizations integrate change management into their overall business strategy, not just IT projects?
Robbie Bullough:
It starts with leadership alignment and continues with clear, transparent communication throughout every phase, from preparation through sustainment. Change management isn’t a one-time task; it’s like a liquid that should flow throughout the organization.
Meg Johnson:
One of the most practical steps any organization can take right now is to equip leaders to lead through change. Build the “change muscle” at all levels so leaders understand their roles, the tools available, and the shared language for talking about change. That foundation makes it easier to activate when new initiatives arise—technical or otherwise.
Q: How should organizations measure success beyond technical metrics?
Meg Johnson:
We start by defining what success looks like early: What percentage of adoption is realistic, how quickly to expect results, and what outcomes truly matter. Then we track awareness, engagement, and capability through surveys and feedback loops. These insights let us adapt our approach in real time, whether by strengthening sponsor visibility or refining communication.
Robbie Bullough:
The feedback loop is critical. It’s not enough to collect feedback—you have to act on it and show people how their input led to change. When employees see that their voices drive decisions, they’re more invested in sustaining success.
Q: What advice would you give healthcare leaders to ensure change is sustainable long after go-live?
Meg Johnson:
Shift away from a “project” mindset. Go-live is just one moment in a longer journey. Adoption happens over time, and it’s fueled by honest feedback, transparency, and celebrating progress. When people see how their work connects to better patient outcomes, that’s what keeps change alive.
Robbie Bullough:
Exactly. Sustainability means managing change through and beyond go-live. These principles apply not just to IT but to any organizational change—mergers, restructures, process redesigns, anything that affects people. If you follow a structured, human-centered framework, you’ll create lasting transformation.
Listen to the Full Conversation
To hear the complete interview with Meg Johnson and Robbie Bullough, click here.
Insight
Realizing the Value of AI Starts With Data Governance and Leadership Support
By Mark Leifer, Data and Analytics Manager
AI dominates healthcare conversations. Vendors are knocking. Leadership is pressured to act. Pilots are sprouting across the industry. EHR vendors like Epic, Meditech, and Oracle are rolling out exciting AI tools that are embedded directly into their platforms.
Whether your organization is adopting those EHR-native tools or building a custom solution, one thing is clear: Data governance is foundational.
Amid the AI buzz, many health systems remain stuck in the proof-of-concept phase, unable to scale or sustain results. Gartner reports that, by 2027, 60% of organizations will fail to achieve the full value of their AI initiatives due to poor data governance.
In my experience, this isn’t a technology failure. It’s because the organization isn’t ready, and leadership hasn’t made data governance a priority.
Without Governance, AI Can’t Deliver Results
Imagine your organization rolls out a shiny new AI tool for clinical decision support. The logic is sound. It integrates with the EHR and the demo wowed the C-suite. But six months in, utilization is low, analysts distrust the data, and compliance wants to know who approved it.
This isn’t hypothetical. In fact, it’s a common pattern. AI stalls not because the tech fails, but because data governance was never embedded in the foundation. Behind that missing foundation is a lack of executive sponsorship.
Governance Needs a Seat at the Leadership Table
If AI is going to succeed in healthcare, data governance can’t live in the shadows. It needs executive backing, visibility, and resources.
Once an organization sets clear, business-aligned goals for data and AI, the next most important success factor is strong executive sponsorship. Ideally, that sponsor is someone with a C-level title — like a CIO, CMIO, or chief data officer — who can connect the dots between business strategy and the operational work of governance.
Modern data governance should emphasize accountability, clear decision-making authority, cultural alignment, and measurable outcomes rather than focusing solely on control. Executive sponsors are critical to bridging those priorities across business and IT. Their role is not to manage the day-to-day, but to model support, prioritize funding, and align governance with organizational goals.
When leaders show up to governance councils, reference it in strategy discussions, and reward good data practices, the signal is clear: This matters.
Culture, Not Control, Is the Real Barrier
Governance must move from fixing data to enabling confident use of data across the enterprise, from “AI as a cool tool” to “AI as a governed system.” Developing a strong data culture happens through modeling, incentives, and stewardship that’s embedded into real workflows. Without that cultural groundwork, even well-designed AI tools will flounder. Teams won’t know who owns the data. Trust will be low. People won’t feel confident using the outputs. Worse, they may not feel safe raising concerns when something looks off.
Build a Coalition, Not a Silo
Executive sponsorship is step one. Step two is building a data governance coalition that spans departments. This coalition — ideally a formal data governance committee — should include IT, clinical leadership, compliance, operations, and analytics. Too often, these groups are working in silos. This structure ensures that governance is positioned as a value enabler and a risk mitigator for AI adoption, rather than bureaucracy.
When it comes to AI, the governance committee should help define approval processes, monitor model performance, and ask questions about transparency, bias, and explainability. But they should also help build buy-in, provide feedback loops, and support training across the organization.
Is Your Culture Ready for AI?
Here are four signs that it may not be:
- No one can clearly answer who owns governance for AI tools.
- A promising AI pilot was shelved due to unclear accountability or lack of trust.
- Data decisions are made in silos or based on influence, not strategy.
- Governance is viewed as red tape, not a strategic capability.
If these sound familiar, you have work to do; but these are fixable problems.
Three Practical Moves To Build Executive-Led Data Governance
If your organization wants better AI outcomes, here’s what I recommend:
- Appoint a C-level sponsor for governance and AI readiness. This person should connect governance to business strategy. Not manage the weeds, but advocate visibly and consistently.
- Stand up a formal data governance committee that includes stakeholders from across the organization. Give it real authority, diverse voices, and a regular meeting cadence.
- Make cultural change part of the plan. Train people, talk about successes, and share stories where good governance led to better outcomes. Help teams see data governance as something that supports their work, not slows it down.
Final Thought
AI won’t transform healthcare if we treat it like a series of disconnected tech pilots. It must be guided by strategy, grounded in governance, and shaped by people who understand the intersection of data, operations, and clinical care. That kind of alignment demands executive leadership, cultural change, and above all, trust. And trust begins with governance.
This article originally appeared in HIStalk.
Insight
6 Ways Revenue Cycle Leaders Can Balance Urgency With Empathy
By Margaret Martin, Managing Director, Revenue Cycle Transformation
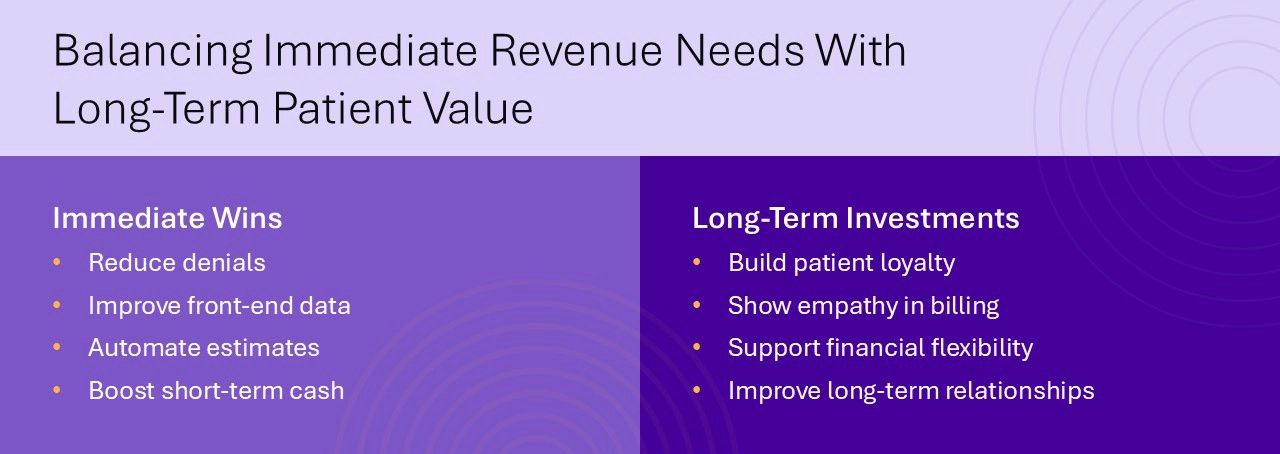
Healthcare organizations are navigating a season of financial uncertainty. With looming Medicaid reimbursement cuts, higher rates of denied claims, and the rising cost of labor and technology, the pressure to deliver short-term financial results has rarely been greater. Yet focusing solely on immediate cost containment can erode patient trust and loyalty. Once lost, these assets are difficult to recover.
To succeed in today’s climate, healthcare leaders must strike a balance: Stabilize revenue performance in the short term while investing in the long-term value of patient relationships. That means leading with empathy, aligning revenue operations with patient expectations, and building a more resilient, patient-centered approach to revenue cycle performance.
Stabilize Financial Performance With Immediate Wins
When budget pressures mount, quick wins are essential. Fortunately, several revenue cycle strategies can yield measurable returns within 12 to 18 months without compromising patient experience.
1. Focus on Denials Management
Denied claims continue to be one of the largest sources of revenue leakage across the industry. Reducing avoidable denials not only improves cash flow, but also reduces administrative burden and staff burnout.
A large academic health system partnered with Tegria to optimize revenue cycle processes after transitioning to a new EHR. Tegria helped minimize financial risks, mitigate challenges, and improve revenue integrity to drive down denials. Over the course of the engagement, more than 1,000 denials were prevented, and auto-accepted secondary claims increased by 321%. Read the case study.
2. Improve Front-End Data Collection
Clean claims begin with clean data. Registration errors, eligibility mismatches, and missing demographics often originate at the front end and ripple downstream. Correcting these issues in real time can eliminate the need for costly rework later.
3. Optimize Patient Estimates and Payment Flexibility
Today’s patients expect clarity and control when it comes to healthcare costs. Organizations that provide upfront estimates and payment plan options are more likely to collect patient responsibility and preserve goodwill.
University of Colorado Health partnered with Tegria to transform their patient estimate process for greater accuracy and transparency. Their solution increased estimates by 6,000% and improved estimate accuracy by 30% to reduce billing surprises for patients. Read the case study.
Invest in Long-Term Patient Relationships
While financial stability is urgent, the path to sustainable growth runs through long-term relationships. Patients who trust their providers are more likely to return, refer others, and engage in their care. Revenue cycle teams play a vital role in shaping that trust.
4. Extend the Patient Relationship Horizon
Viewing patients through a transactional lens can be shortsighted. Instead, organizations should consider patient lifetime value: the total revenue, impact, and loyalty a patient brings over time.
Accurate billing, proactive communication, and streamlined financial touchpoints all contribute to a positive experience. Investments that build patient trust today can yield years of future engagement.

5. Show Empathy in Billing Practices
Medical debt is a leading source of financial hardship in the U.S., and patients often delay or avoid care due to cost concerns. Revenue cycle teams have the power to change that narrative by leading with empathy.
Simple actions like offering income-based discounts, flexible payment terms, and accessible billing statements can transform the patient financial experience, resulting in loyal patients who return year after year.
6. Recognize the Impact of Financial Stress on Trust
Financial stress impacts patients beyond their wallets, by eroding trust in the entire healthcare system. When patients are surprised by a bill or feel dismissed when they ask for help, they’re less likely to seek care in the future.
To prevent this, healthcare organizations must integrate access, care, and financial functions into one coordinated experience. When patient access staff, clinicians, and billing teams work together, patients benefit from clear expectations and compassionate support.
Building an Integrated Approach
Silos between financial, operational, and clinical departments often stand in the way of progress. To deliver a better financial experience for patients, organizations must unite these functions around shared goals.
That includes:
- Sharing real-time data across access, billing, and clinical systems
- Training staff to speak the same language of patient empathy
- Leveraging technology to automate routine tasks and flag issues early
- Embedding empathy and equity into every financial touchpoint
Tegria partners with healthcare organizations to design and implement these integrated approaches, resulting in stronger revenue performance and improved patient loyalty.
Conclusion: Sustainable Growth Requires a Balanced Approach
In times of financial stress, it’s tempting to focus on short-term gains alone. But healthcare organizations that also prioritize long-term patient relationships will emerge stronger.
Immediate improvements in denials management, front-end workflows, and patient estimates can create fast, measurable impact. At the same time, embedding empathy into billing practices builds trust that pays dividends far beyond the current fiscal year.
Tegria helps organizations align revenue cycle performance with patient-centered care—so you don’t have to choose between financial health and human connection.
Insight
4 Key Takeaways From MEDITECH LIVE 2025
At Tegria, we believe healthcare transformation happens when operations and technology evolve together. That belief was reinforced at MEDITECH LIVE 2025, where discussions centered on how health systems can modernize in practical, measurable ways while keeping patients and clinicians at the center.

1. Modernization is no longer optional.
Hospitals using legacy platforms finding that lack of enhancements and support is accelerating their move to MEDITECH-as-a-Service (MaaS) as some vendors wind down support of older versions. This underscores a broader industry trend: health systems cannot afford to stand still. Modernization is about more than upgrading to the latest version—it’s about future-proofing the operating model.
2. AI is moving from concept to embedded strategy.
We heard keen interest in AI, not just through MEDITECH partners, but also in how Expanse is rolling out agentic features to weave AI into clinical and operational workflows. This reflects what we see across the industry: Organizations aren’t chasing AI for its own sake. Instead, leaders are asking how AI can meaningfully improve clinician satisfaction, simplify the revenue cycle, and elevate the patient experience.
3. Expanse upgrades are unlocking innovation.
Many organizations are advancing from Expanse 2.1 to 2.2, enabling them to adopt the latest interoperability features and intelligent automation. Clients are already using Expanse to achieve CHIME Most Wired status, simplify revenue cycle processes, and apply AI in ambulatory care settings.

4. Community and collaboration fuel progress.
From packed Immersive Track sessions to a lively networking reception, the energy at this year’s event made it clear that Expanse is more than a platform. It’s an ecosystem where providers, technology partners, and service organizations like Tegria come together to reimagine care delivery.
Our Perspective on MEDITECH LIVE 2025
Healthcare leaders must balance financial pressures, clinician burnout, and growing patient expectations. The organizations that will thrive are those embracing modern EHR platforms while aligning technology with operational priorities. At Tegria, we’re proud to guide clients on that journey. Learn more about our MEDITECH EHR Services.
Insight
Your Guide to CMS-0057-F Compliance
Don’t fall behind: How payers can prepare for 2026 and 2027 compliance deadlines
CMS-0057-F at a Glance
The Interoperability and Prior Authorization Final Rule (CMS-0057-F) introduced new requirements for Medicare Advantage, Medicaid, CHIP, and Qualified Health Plan (QHP) payers on the Federally Facilitated Exchange (FFE). The rule aims to reduce delays in care, improve data exchange, and enhance transparency.
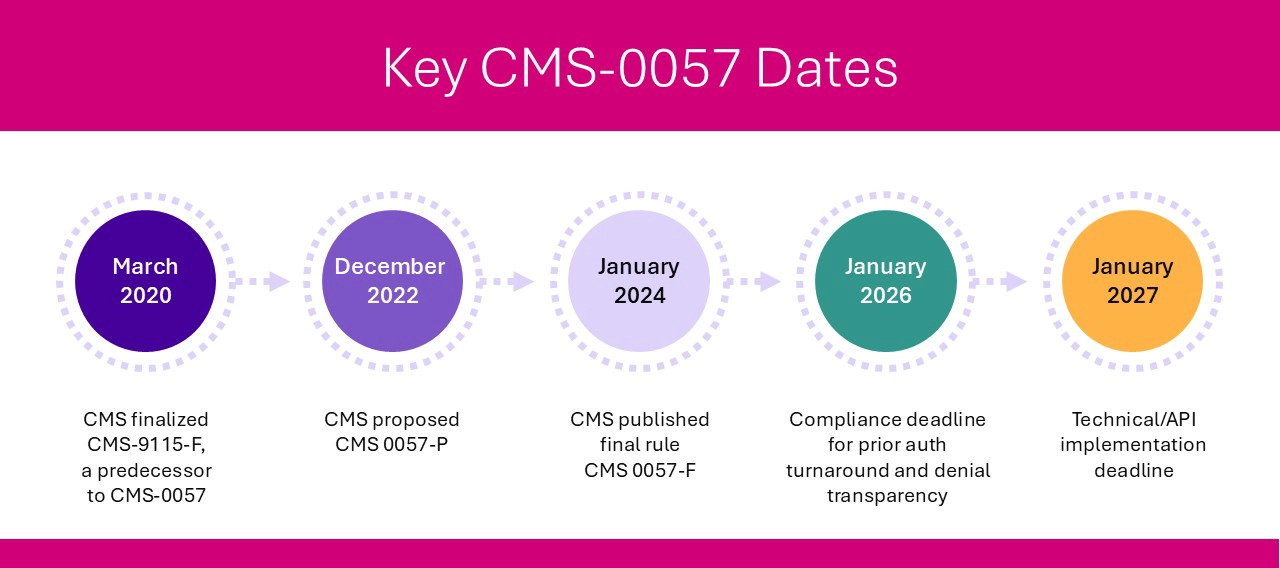
Affected payers must comply with operational changes by January 1, 2026, and meet FHIR API implementation and reporting requirements by January 1, 2027. To prepare, payers should focus on four key categories: data exchange between payers, enhanced patient data access, interoperability with in-network providers, and streamlined prior authorization processes.
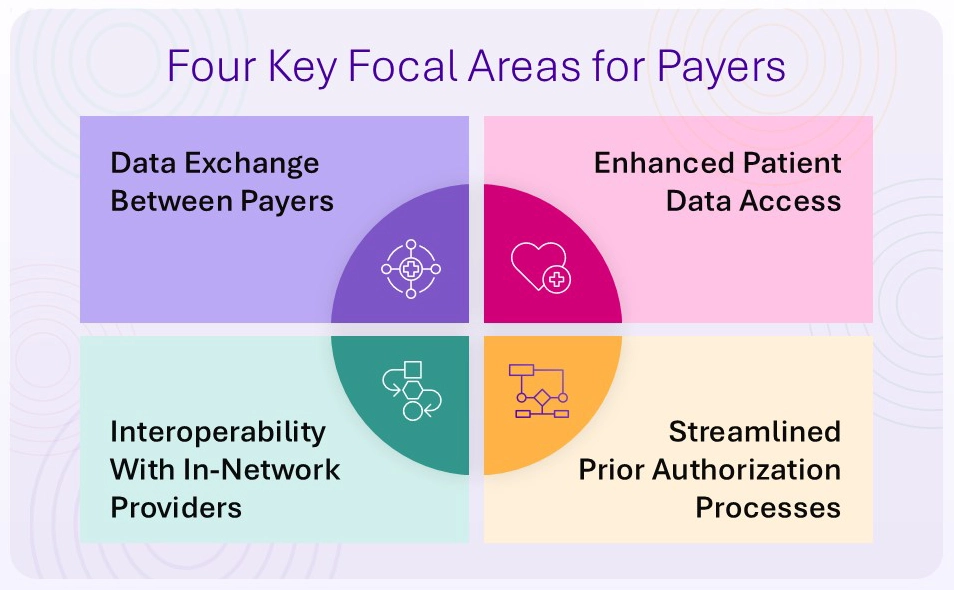
Four CMS-0057-F Requirements Payers Must Address
1. Payer-to-Payer Data Exchange
To support care continuity and reduce duplication, payers must exchange patient data—such as claims, encounters, and prior authorization decisions—when a member switches plans. This exchange must happen via a FHIR-based API and at the member’s request.
- For members with concurrent coverage, payers must share relevant data at least quarterly.
- Financial data is not required to be exchanged.
- The goal: a longitudinal health record that follows the patient from plan to plan.
2. Expanded Patient Access API
Building on the 2020 CMS interoperability rule, CMS-0057-F requires payers to expand the Patient Access API to include prior authorization information.
This means patients must be able to access:
- Whether prior authorization is required for a specific item or service
- Documentation requirements
- Status and decisions on prior authorization requests
This supports informed decision-making and greater transparency for patients managing their own care.
3. Provider Access API
To support value-based care and timely treatment decisions, payers must share clinical and administrative data with in-network providers via a new Provider Access API. This includes:
- Claims and encounter data
- Prior authorization request statuses and decisions
Importantly, patients must have the option to opt out of this data sharing and must be notified of this choice.
4. Prior Authorization API and Operational Improvements
CMS-0057-F introduces both technical and operational requirements to improve the speed, transparency, and automation of prior authorization workflows.
API Requirements (due by January 1, 2027):
Payers must implement a FHIR-based Prior Authorization API that allows providers to:
- Identify whether prior authorization is needed
- Submit requests and supporting documentation electronically
- Receive prior authorization decisions through EHRs or practice management systems
The ANSI X12 278 standard continues to be supported for back-end transmission.
Operational Requirements (effective January 1, 2026):
- Faster turnaround times:
- Urgent requests: within 72 hours
- Standard requests: within 7 calendar days (down from 14)
- Detailed denial reasons: must be included to enable quick resubmissions
- Five-year data availability: prior authorization history must be retained and shared upon request
Public reporting: beginning in 2027, payers must publish prior authorization metrics including total requests, approvals, denials, and average processing times. These updates represent major CMS regulatory changes designed to speed up approvals and create consistency across payers.
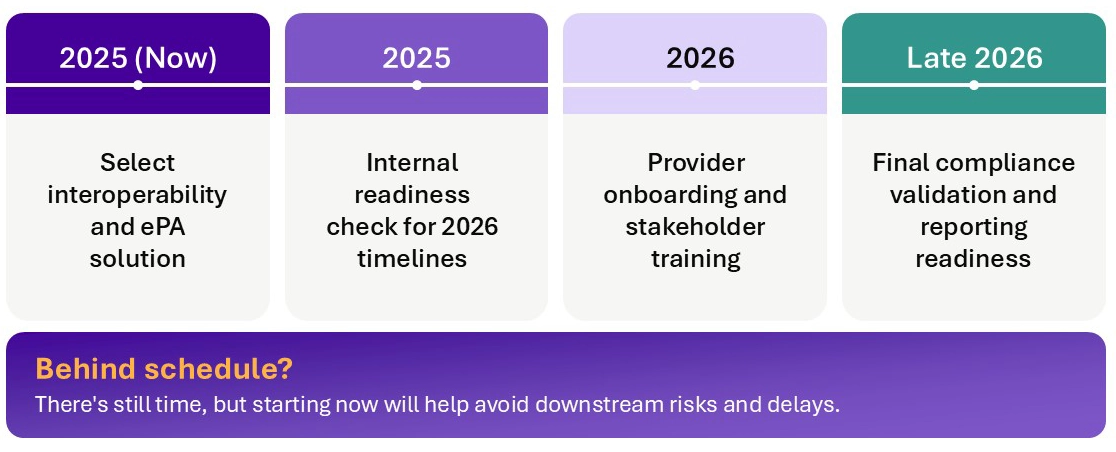
Planning Milestones for Payers
Looking for more provider-focused CMS-0057-F guidance?
How To Plan for Success
With multiple CMS-0057-F deadlines approaching, payers need a focused strategy for both compliance and long-term value creation. Key steps include:
Choose the right interoperability solution
Ensure your platform:
- Supports all four required APIs (Patient Access, Provider Access, Payer-to-Payer, Prior Authorization)
- Meets HL7® FHIR® technical standards
- Aligns with your data infrastructure and provider network needs
Build the right team
Bring together cross-functional experts in:
- Electronic prior authorization and FHIR APIs
- Business intelligence and metrics reporting
- Provider relations and onboarding
- Claims and eligibility systems
Think beyond compliance
Leverage interoperability to improve care coordination, reduce administrative burden, and enhance member and provider experience. For example:
- Automated chart retrieval and electronic release of information (ROI) can accelerate medical necessity reviews.
- Integration with downstream systems can reduce redundant work and manual handoffs.
Collaborate early with providers
Understand provider workflows and explain how your APIs can reduce their administrative overhead. Provider buy-in will be essential to realizing the intended benefits of interoperability.
Explore detailed guidance for payers and providers.
The Bottom Line
CMS-0057-F sets the stage for a more transparent, efficient, and interoperable healthcare system. For payers, these changes are not just a regulatory burden—they’re an opportunity to modernize infrastructure, strengthen provider partnerships, and enhance the member experience.
Is your CMS-0057 strategy ready for key deadlines? The time to act is now. Whether you’re on track or falling behind, we’re here to help you meet your goals. Contact us to speak with an expert.
Wherever you are on your interoperability journey, Tegria can help.

Whether you’re just getting started, ready to move to the cloud, or somewhere in between, we’ll meet you where you are, guiding you on your journey toward achieving operational readiness, collaborative provider payer relationships, and realization of ROI.
For more focused guidance on CMS-0057-F readiness, download our checklist.
Insight
5 Technology Trends Shaping Payer Strategy
By Stephanie Ngo, Managing Director, Payer
As 2026 comes into focus, health plans are accelerating innovation. Vendors are focused on modernizing tools, platforms, and processes to enhance transparency, collaboration, and experiences. Whether starting small or pursuing enterprise-wide transformation, payers are seeing more options—and more urgency—than ever.
Here are five key trends impacting payer strategy, based on what we’re seeing in the market and hearing from health plan leaders:
1. Platform-Based Transformation Gains Traction and Depth
More health plans are choosing platforms and partners that can support everything from care management to claims processing. Some begin with targeted rollouts, while others are going all-in with enterprise implementations that include provider data management, portals, and interoperability. To support this shift, technology vendors are actively expanding their offerings to make comprehensive implementations more feasible for health plans.
2. New Functionality Elevate Compliance, Experience, and Insight
Functionality is evolving across the board to meet payer needs. Some of the most compelling developments include:
- Quality collaboration between payers and providers to measure and manage cost and quality.
- Provider directory tools that connect members with providers.
- Employer and broker portals with integrated payment and reporting capabilities.
- Interoperability (interop) enhancements supporting compliance with CMS-0057 data exchange requirements.
- Price transparency capabilities to meet regulatory requirements and empower members’ decision-making.
- Member experience upgrades offering digital self-service and omnichannel options to unify call center, mobile, and digital engagement.
- Operational dashboards that offer real-time benchmarking and insights into key functions and performance metrics.
- Provider data management solutions that clean and maintain critical provider information.
- Advanced intake tools that use OCR (optical character recognition) to eliminate manual processes.
These enhancements represent a meaningful shift toward payer functionality that’s more agile, member-centered, and compliance-ready.
3. AI Takes Center Stage
AI continues to dominate conversations around payer transformation. Across the industry, organizations are exploring how AI can reduce friction, unlock insights, and improve both speed and accuracy. Flexible pricing models and bundled solutions are making AI more accessible, encouraging phased adoption that aligns with organizational readiness.
4. Tools Must Deliver Real-World Value for Payers
While AI often feels like hype, we’re seeing real, value-generating applications across key payer workflows:
- AI for prior authorization workflows to ease the submission process for providers, speeding decisions for payers while increasing transparency and reducing administrative burden for everyone.
- Risk adjustment that surfaces accurate and comprehensive risk capture supported by clinical documentation that is shared between payer and provider.
- Advanced analytics and reporting tools empowering end users to easily turn raw data into strategic insight via generative AI.
- AI for claims processing that automates high-volume tasks to improve speed and accuracy.
These tools are designed not just for experimentation but for real-world operational improvement. And as they mature, we expect them to become integral to how modern health plans work.
5. Flexible, Modular Strategies Are Winning
As payer strategy evolves, vendors are ready to meet payers where they are. The path to implementation doesn’t have to be all or nothing—many plans are pursuing a phased approach, starting with targeted use cases or a limited tech stack and expanding over time.
Bottom Line
As health plans navigate a complex and fast-changing landscape, technology decisions are becoming more critical. Organizations that embrace flexibility, interoperability, and intelligent automation are better positioned to reduce costs, satisfy members, and meet regulatory demands.
Whether you’re exploring CRM, utilization management modernization, or full-stack platform consolidation, these trends offer a roadmap for what’s possible—and what’s next.
Strengthen Your Payer Strategy With Tegria
Insight
Beyond Go-Live: 6 Continuous Optimization Strategies for Epic
Implementation Isn’t the Finish Line
Going live with Epic marks a major milestone that often follows years of planning, preparation, and investment. For most organizations, however, the real work begins after the initial launch. Without a plan for continuous optimization, momentum can fade, Epic’s capabilities may be underused, and opportunities for gains in efficiency, revenue, and patient care can be lost.
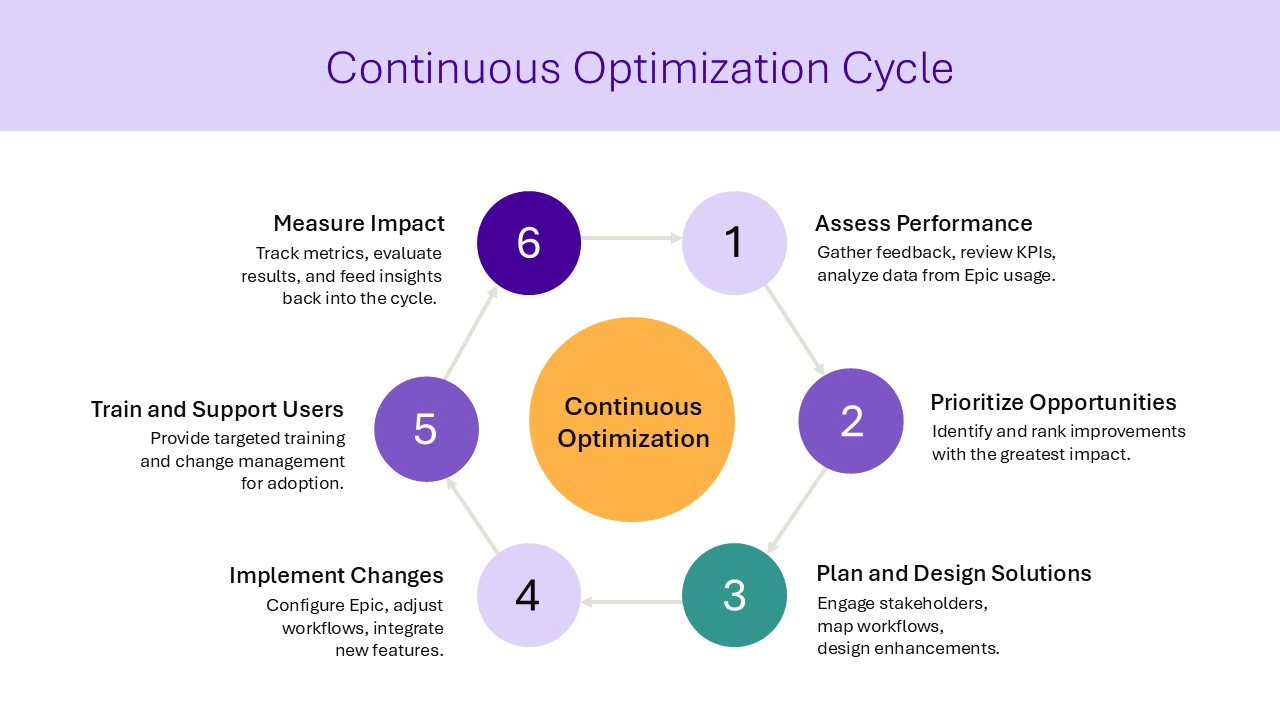
Tegria has supported some of the most complex Epic implementations in the country, embedding teams that work side by side with clients to sustain progress, adapt to evolving needs, and achieve long-term return on investment. From refining clinical workflows to expanding data and analytics capabilities, our experience shows that the most successful organizations approach optimization as an ongoing discipline rather than a one-time event.
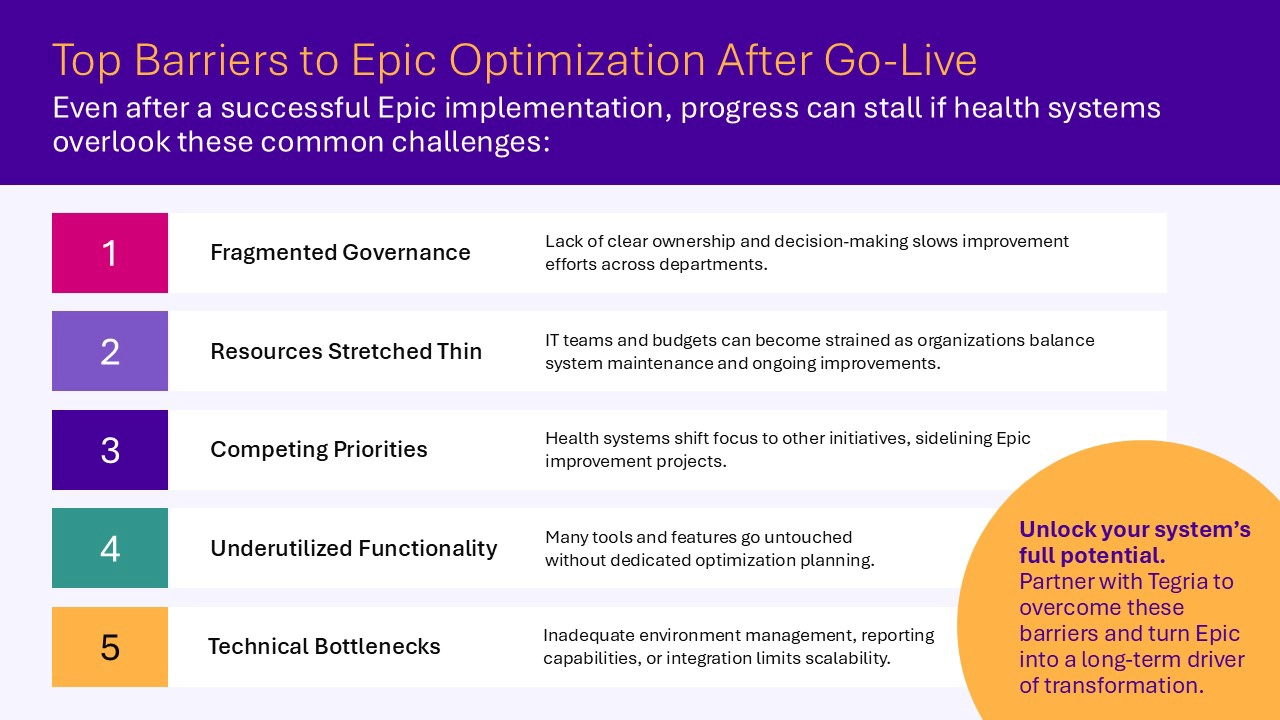
Why Continuous Optimization Matters
Even the best-planned go-lives reveal gaps in workflows, user adoption, and system performance. In the early post-live period, these challenges can be masked by the focus on system stabilization. Over time, health systems often face familiar issues: workflow misalignment, inconsistent user adoption, reporting gaps, and technical bottlenecks.
Beyond stabilization, the healthcare environment continues to evolve. New regulatory requirements, changing payment models, system upgrades, and shifting patient expectations all require ongoing refinement of Epic environments. Governance structures that worked during implementation may need to be redesigned for long-term decision-making and prioritization.
Organizations that maintain performance and realize sustained value share a common trait: They take a proactive, data-driven approach to optimization. Continuous engagement with stakeholders, regular performance monitoring, and targeted improvements all help drive efficiency, clinician satisfaction, and better patient outcomes.
Strategic Areas of Focus for Optimization
The most effective optimization strategies are targeted and measurable, built on performance data from your Epic system. By focusing on the following areas, health systems can achieve sustained improvements and measurable returns.
Clinical and Operational Alignment
Optimization begins with aligning clinical workflows to operational goals. This requires ongoing engagement with clinicians to adapt Epic to their needs, reduce administrative burden, and improve patient care. Physician informatics programs can enhance usability, streamline documentation, and give clinicians more time with patients. Capacity management tools help align clinical supply with patient demand, improving throughput and reducing delays.
Epic EHR Optimization Saves Clinician Time, Increases Efficiency
Tegria cut In Basket messages by nearly 1,000 per day and minimized clicks for providers, staff, and coders.
Revenue Cycle Optimization
Financial performance is directly tied to the accuracy and efficiency of clinical workflows. Post-go-live, organizations often find opportunities to better integrate front-end and back-end processes.
Designing a Single Billing Office, improving the patient financial experience, and strengthening charge capture can deliver measurable revenue gains while supporting patient satisfaction.
Strategic Revenue Integrity Improvements Generate $19.4 Million
Tegria optimized charge capture, automation, reconciliation, and charge description master governance to prevent lost revenue.
Training and Change Management
Technology alone does not ensure success. Staff turnover, role changes, and system updates create a constant need for training. Without it, user adoption declines and optimization results can diminish.
An effective training program includes ongoing education for new hires, credentialing for trainers, and refreshers tied to system upgrades. A well-maintained training environment ensures teams are prepared for new features and workflows.
UW Medicine Transforms Initial EHR Education With Amplifire
UW Medicine slashed training time for nurses by 75% and reduced training time for providers by 50% using an adaptive learning platform.
Data Analytics and Reporting Support
Epic holds a wealth of operational and clinical data; but without the right reporting and analytics approach, its potential remains untapped. Optimization includes building reliable reporting tools, ensuring data accuracy, and delivering timely insights that support decision-making.
Business Intelligence teams can meet ongoing operational and clinical reporting needs while advancing analytics maturity, from descriptive reports to predictive modeling and value-based care initiatives.
Technology and Infrastructure Support
Strong technical foundations are essential for successful optimization. This includes environment management, upgrade planning, and integration with other systems.
Efforts may involve biomedical device integration, third-party system connections such as lab systems or Capsule, and improvements to environment synchronization processes. Proactive management reduces bottlenecks and prepares the system to scale as the organization grows.
EpicCare Ambulatory Specialty Sprints Increase User Satisfaction, Secure Revenue
An academic health system in the Midwest created an EpicCare Ambulatory sprint program to reduce a backlog of application enhancement requests.
Integrated Readiness Planning
Live organizations often expand services, add new locations, or introduce additional Epic modules. Each change requires operational and technical readiness.
Integrated readiness planning supports major events like CFO Summits, Clinic Manager Days, and Patient Flow Days, and creates repeatable processes for onboarding new services, clinics, and staff. Thorough planning minimizes disruption and accelerates adoption.
Creating a High-Performing Epic PMO To Scale Implementations
Tegria helped the University of Colorado Health scale Epic implementations and develop a strong internal Project Management Office.
Tegria’s Optimization Framework
Tegria views continuous optimization as a sustained partnership that adapts to evolving needs. Our framework includes:
- Advisory Services: Strategic guidance on governance, workflow design, and long-term planning.
- Build and Integration: Technical expertise for Epic configuration, environment management, and third-party integrations.
- Support Services: Role-based Tier 2 and Tier 3 support to expand capacity and address issues efficiently.
- Analytics Enablement: Development of operational and clinical reporting capabilities to inform decisions.
- Embedded Teams: Consultants, analysts, informaticists, and trainers who work alongside client teams to ensure adoption.
This flexible model ensures that optimization efforts remain aligned with each organization’s goals and priorities.
Building a Culture of Continuous Improvement
Sustainable optimization depends on a culture that embraces ongoing improvement. This means embedding optimization into governance structures, maintaining visibility into performance metrics, and making decisions based on data.
Regular optimization workgroups keep initiatives on track, while monitoring key performance indicators—such as provider satisfaction, throughput times, and revenue cycle metrics—helps identify new opportunities.
Keeping pace with Epic upgrades is equally important. Falling behind can limit access to new functionality and create technical debt. Leveraging Epic’s AnyTime Notes and following upgrade readiness plans ensure the system continues to evolve with the organization’s needs.
Achieving Epic Gold Star Recognition With Ongoing Support
Montage Health reduced Epic OPA volume by 58% and completed 13 Epic upgrades with Tegria’s support.
Conclusion: Realizing the Full Value of Epic
The launch of Epic is a significant milestone, but long-term success comes from what happens afterward. A proactive, structured approach to optimization can enhance workflows, strengthen financial performance, improve satisfaction for both patients and providers, and help organizations adapt to a changing healthcare landscape.
Tegria partners with health systems to design and implement optimization strategies that align with organizational goals, deliver measurable value, and ensure Epic remains a catalyst for transformation. From advisory and technical expertise to embedded support, we help clients build the foundation for sustained success.
Ready to take your Epic environment beyond go-live?
Contact us to start planning your post-live optimization roadmap.
Epic is a trademark of Epic Systems Corporation.
Insight
Designing Better Care Models With Virtual Nursing: 5 Key Webinar Takeaways
The American Hospital Association’s recent webinar, “From Complexity to Clarity: Mapping Virtual Nursing for Change,” featured leaders from Froedtert ThedaCare and Tegria. The conversation explored how virtual nursing, when thoughtfully designed, can address workforce challenges, improve care team experience, and strengthen care delivery.
If you missed the session, here are five key takeaways that stood out—each pointing to real opportunities for healthcare organizations to rethink care models and invest in patient and staff experience.
1. Virtual Nursing Can Help Bridge the Workforce Gap
The nursing shortage continues to strain care teams. National RN vacancy rates are nearing 10%, and nurses under age 35 are leaving the profession at four times the rate of their older peers. These trends have led to a growing “complexity gap” as experienced nurses exit the workforce and less experienced staff step in.
Virtual nursing offers a way to close that gap by supplementing bedside care with remote clinical support. Whether supporting new nurses during admissions or providing real-time surveillance, virtual nurses can play a vital role in creating a more sustainable care model.
2. Transforming Care Starts With Systemwide Thinking
Rather than focusing on isolated fixes, the speakers emphasized the need for systemic thinking. Every care experience is shaped by interconnected processes, tools, and people. Misaligned workflows, technology gaps, and siloed roles can lead to burnout and inefficiencies—even when intentions are good.
Redesigning care models with the full system in mind helps teams address root causes rather than symptoms. When workflows are designed around both patient needs and staff realities, teams are better equipped to deliver safe, high-quality care.
3. Visual Tools Bring Clarity to Complex Problems
To support this kind of transformation, Tegria introduced experience alignment tools such as journey maps and service blueprints. These tools help organizations visualize current-state pain points, identify improvement opportunities, and align on shared goals, which can include business objectives, North Stars, experience goals, and operational metrics.
By capturing both the emotional and operational aspects of patient and staff experience, these tools help leaders and frontline teams work together more effectively. They also make it easier to prioritize changes and socialize new workflows across departments. Equally important, they bring analytical and systematic rigor to complex problem-solving—functioning as a kind of service “Rosetta stone” that aligns diverse teams around a shared view of the system. By making abstract and multi-layered care services visible and modular, these tools help organizations examine, design, and improve them in a structured way, reducing risk and cost while supporting sustainable transformation.
4. Virtual Nursing Is Scalable—Even for Smaller Systems
One theme that emerged clearly from the conversation: You don’t need a large budget or advanced infrastructure to start. Froedtert Thedacare, for example, began testing virtual admissions support with a simple phone-based process before investing in higher-tech solutions.
Even small steps can yield meaningful results, such as improved workflow, reduced documentation burden, or better mentorship for new nurses. With the right care model and team-based approach, organizations of all sizes can find ways to make virtual nursing work for them.
Virtual nursing isn’t just a tech solution for Froedtert ThedaCare. It’s a strategic workforce initiative designed to support our teams, reduce burnout, and reimagine the future of care.
ERIKA SMITHExecutive Director of Transformation and Integration, Froedtert ThedaCare
5. Designing for Real People Creates Stronger Systems
The webinar introduced four fictional nurse personas—Marie, Jen, Toby, and Betsy—to reflect the challenges and opportunities nurses face throughout their careers. Each story highlighted how virtual nursing and thoughtful workflow design can support experienced leaders, mid-career mentors, early-career learners, and veterans transitioning out of bedside roles.
Designing around these needs isn’t just a creative exercise. It’s a practical approach to retaining staff, reducing burnout, and ensuring consistent, high-quality care. When people feel supported, they stay, grow, and contribute more fully to their teams.
Ready to improve access and elevate experience across your health system?
Tegria partners with healthcare organizations to modernize care delivery, streamline patient and staff experiences, and implement sustainable solutions that drive better outcomes.