Insight
Your Guide to CMS-0057-F Compliance
Don't fall behind: How payers can prepare for 2026 and 2027 compliance deadlines
This Article Covers
CMS-0057-F at a Glance
The Interoperability and Prior Authorization Final Rule (CMS-0057-F) introduced new requirements for Medicare Advantage, Medicaid, CHIP, and Qualified Health Plan (QHP) payers on the Federally Facilitated Exchange (FFE). The rule aims to reduce delays in care, improve data exchange, and enhance transparency.
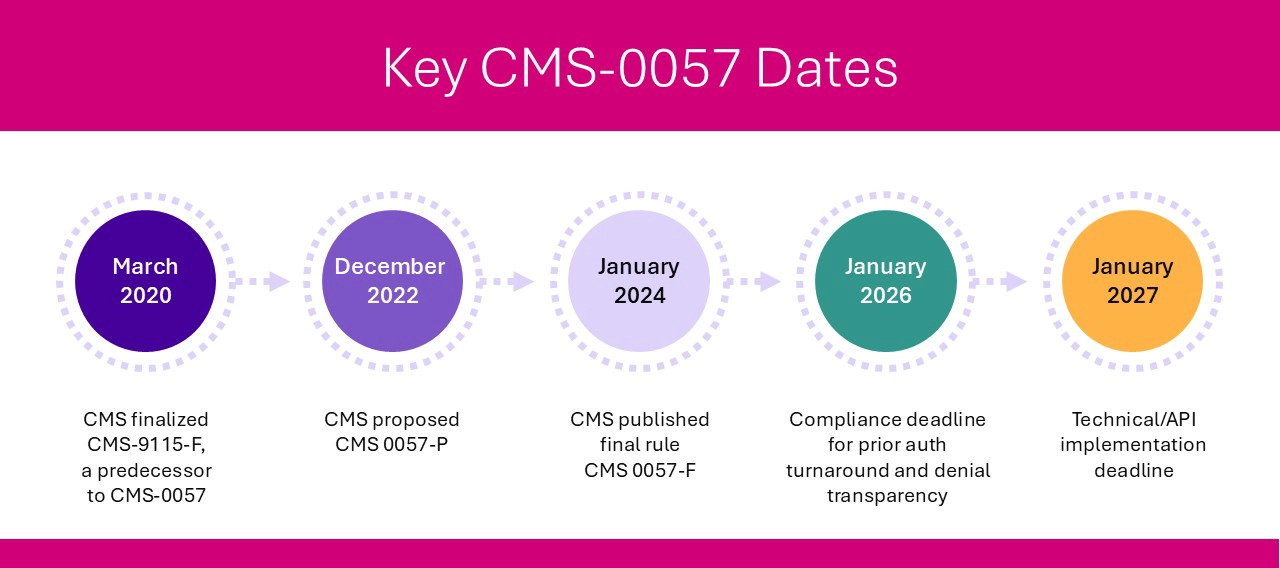
Affected payers must comply with operational changes by January 1, 2026, and meet FHIR API implementation and reporting requirements by January 1, 2027. To prepare, payers should focus on four key categories: data exchange between payers, enhanced patient data access, interoperability with in-network providers, and streamlined prior authorization processes.
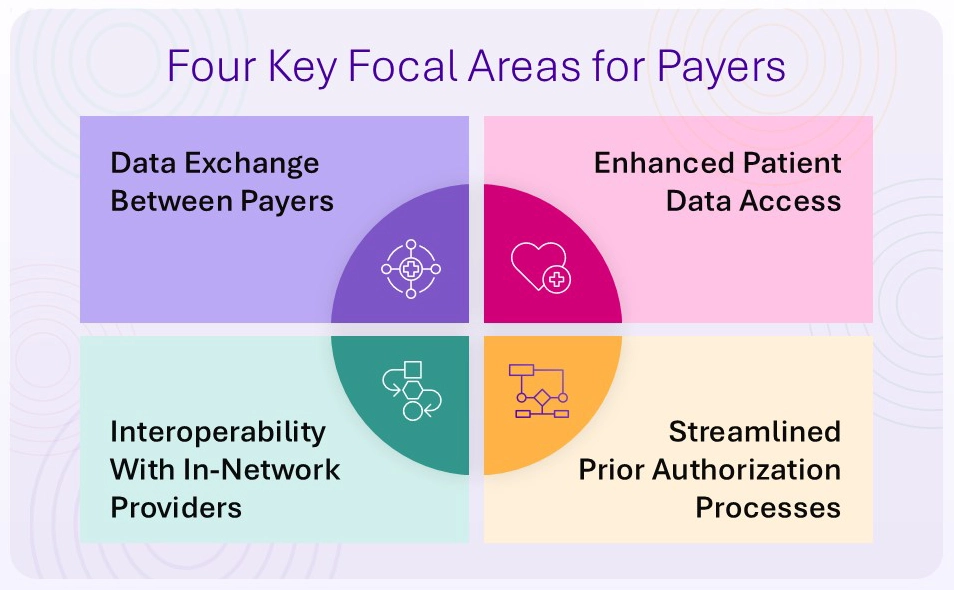
Four CMS-0057-F Requirements Payers Must Address
1. Payer-to-Payer Data Exchange
To support care continuity and reduce duplication, payers must exchange patient data—such as claims, encounters, and prior authorization decisions—when a member switches plans. This exchange must happen via a FHIR-based API and at the member’s request.
- For members with concurrent coverage, payers must share relevant data at least quarterly.
- Financial data is not required to be exchanged.
- The goal: a longitudinal health record that follows the patient from plan to plan.
2. Expanded Patient Access API
Building on the 2020 CMS interoperability rule, CMS-0057-F requires payers to expand the Patient Access API to include prior authorization information.
This means patients must be able to access:
- Whether prior authorization is required for a specific item or service
- Documentation requirements
- Status and decisions on prior authorization requests
This supports informed decision-making and greater transparency for patients managing their own care.
3. Provider Access API
To support value-based care and timely treatment decisions, payers must share clinical and administrative data with in-network providers via a new Provider Access API. This includes:
- Claims and encounter data
- Prior authorization request statuses and decisions
Importantly, patients must have the option to opt out of this data sharing and must be notified of this choice.
4. Prior Authorization API and Operational Improvements
CMS-0057-F introduces both technical and operational requirements to improve the speed, transparency, and automation of prior authorization workflows.
API Requirements (due by January 1, 2027):
Payers must implement a FHIR-based Prior Authorization API that allows providers to:
- Identify whether prior authorization is needed
- Submit requests and supporting documentation electronically
- Receive prior authorization decisions through EHRs or practice management systems
The ANSI X12 278 standard continues to be supported for back-end transmission.
Operational Requirements (effective January 1, 2026):
- Faster turnaround times:
- Urgent requests: within 72 hours
- Standard requests: within 7 calendar days (down from 14)
- Detailed denial reasons: must be included to enable quick resubmissions
- Five-year data availability: prior authorization history must be retained and shared upon request
Public reporting: beginning in 2027, payers must publish prior authorization metrics including total requests, approvals, denials, and average processing times. These updates represent major CMS regulatory changes designed to speed up approvals and create consistency across payers.
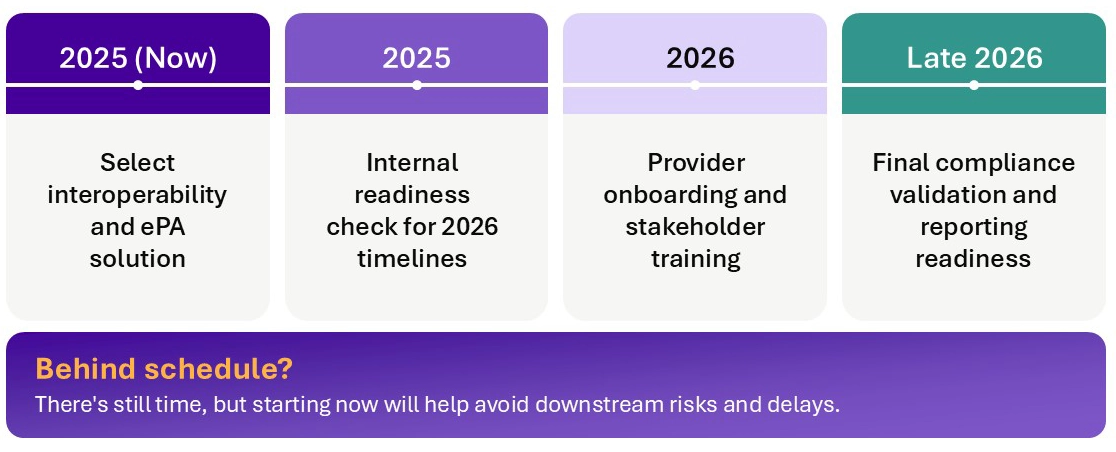
Planning Milestones for Payers
Looking for more provider-focused CMS-0057-F guidance?
How To Plan for Success
With multiple CMS-0057-F deadlines approaching, payers need a focused strategy for both compliance and long-term value creation. Key steps include:
Choose the right interoperability solution
Ensure your platform:
- Supports all four required APIs (Patient Access, Provider Access, Payer-to-Payer, Prior Authorization)
- Meets HL7® FHIR® technical standards
- Aligns with your data infrastructure and provider network needs
Build the right team
Bring together cross-functional experts in:
- Electronic prior authorization and FHIR APIs
- Business intelligence and metrics reporting
- Provider relations and onboarding
- Claims and eligibility systems
Think beyond compliance
Leverage interoperability to improve care coordination, reduce administrative burden, and enhance member and provider experience. For example:
- Automated chart retrieval and electronic release of information (ROI) can accelerate medical necessity reviews.
- Integration with downstream systems can reduce redundant work and manual handoffs.
Collaborate early with providers
Understand provider workflows and explain how your APIs can reduce their administrative overhead. Provider buy-in will be essential to realizing the intended benefits of interoperability.
Explore detailed guidance for payers and providers.
The Bottom Line
CMS-0057-F sets the stage for a more transparent, efficient, and interoperable healthcare system. For payers, these changes are not just a regulatory burden—they’re an opportunity to modernize infrastructure, strengthen provider partnerships, and enhance the member experience.
Is your CMS-0057 strategy ready for key deadlines? The time to act is now. Whether you’re on track or falling behind, we’re here to help you meet your goals. Contact us to speak with an expert.
Wherever you are on your interoperability journey, Tegria can help.

Whether you’re just getting started, ready to move to the cloud, or somewhere in between, we'll meet you where you are, guiding you on your journey toward achieving operational readiness, collaborative provider payer relationships, and realization of ROI.