Insight
Designing Better Care Models With Virtual Nursing: 5 Key Webinar Takeaways
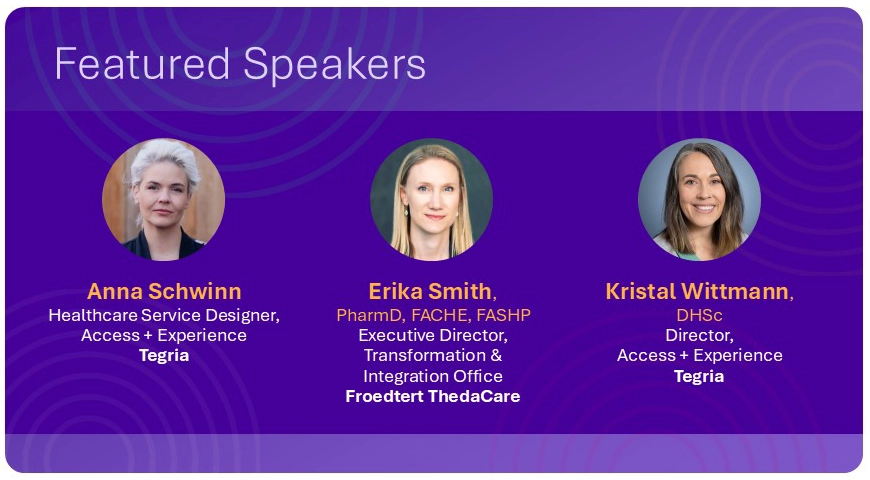
The American Hospital Association’s recent webinar, “From Complexity to Clarity: Mapping Virtual Nursing for Change,” featured leaders from Froedtert ThedaCare and Tegria. The conversation explored how virtual nursing, when thoughtfully designed, can address workforce challenges, improve care team experience, and strengthen care delivery.
If you missed the session, here are five key takeaways that stood out—each pointing to real opportunities for healthcare organizations to rethink care models and invest in patient and staff experience.
1. Virtual Nursing Can Help Bridge the Workforce Gap
The nursing shortage continues to strain care teams. National RN vacancy rates are nearing 10%, and nurses under age 35 are leaving the profession at four times the rate of their older peers. These trends have led to a growing “complexity gap” as experienced nurses exit the workforce and less experienced staff step in.
Virtual nursing offers a way to close that gap by supplementing bedside care with remote clinical support. Whether supporting new nurses during admissions or providing real-time surveillance, virtual nurses can play a vital role in creating a more sustainable care model.
2. Transforming Care Starts With Systemwide Thinking
Rather than focusing on isolated fixes, the speakers emphasized the need for systemic thinking. Every care experience is shaped by interconnected processes, tools, and people. Misaligned workflows, technology gaps, and siloed roles can lead to burnout and inefficiencies—even when intentions are good.
Redesigning care models with the full system in mind helps teams address root causes rather than symptoms. When workflows are designed around both patient needs and staff realities, teams are better equipped to deliver safe, high-quality care.
3. Visual Tools Bring Clarity to Complex Problems
To support this kind of transformation, Tegria introduced experience alignment tools such as journey maps and service blueprints. These tools help organizations visualize current-state pain points, identify improvement opportunities, and align on shared goals, which can include business objectives, North Stars, experience goals, and operational metrics.
By capturing both the emotional and operational aspects of patient and staff experience, these tools help leaders and frontline teams work together more effectively. They also make it easier to prioritize changes and socialize new workflows across departments. Equally important, they bring analytical and systematic rigor to complex problem-solving—functioning as a kind of service “Rosetta stone” that aligns diverse teams around a shared view of the system. By making abstract and multi-layered care services visible and modular, these tools help organizations examine, design, and improve them in a structured way, reducing risk and cost while supporting sustainable transformation.
4. Virtual Nursing Is Scalable—Even for Smaller Systems
One theme that emerged clearly from the conversation: You don’t need a large budget or advanced infrastructure to start. Froedtert Thedacare, for example, began testing virtual admissions support with a simple phone-based process before investing in higher-tech solutions.
Even small steps can yield meaningful results, such as improved workflow, reduced documentation burden, or better mentorship for new nurses. With the right care model and team-based approach, organizations of all sizes can find ways to make virtual nursing work for them.
Virtual nursing isn’t just a tech solution for Froedtert ThedaCare. It’s a strategic workforce initiative designed to support our teams, reduce burnout, and reimagine the future of care.
ERIKA SMITHExecutive Director of Transformation and Integration, Froedtert ThedaCare
5. Designing for Real People Creates Stronger Systems
The webinar introduced four fictional nurse personas—Marie, Jen, Toby, and Betsy—to reflect the challenges and opportunities nurses face throughout their careers. Each story highlighted how virtual nursing and thoughtful workflow design can support experienced leaders, mid-career mentors, early-career learners, and veterans transitioning out of bedside roles.
Designing around these needs isn’t just a creative exercise. It’s a practical approach to retaining staff, reducing burnout, and ensuring consistent, high-quality care. When people feel supported, they stay, grow, and contribute more fully to their teams.
Ready to improve access and elevate experience across your health system?
Tegria partners with healthcare organizations to modernize care delivery, streamline patient and staff experiences, and implement sustainable solutions that drive better outcomes.