Resource
Medicaid Site Visits Services and Support
Optimize provider credentialing processes to meet NCQA requirements and health plan goals
Efficient, accurate, and timely provider credentialing site visits are critical to maintaining compliance with state Medicaid contracts, NCQA, and Centers for Medicare & Medicaid Services (CMS) requirements. Tegria’s team of registered nurse clinical surveyors and administrative support staff can help optimize existing workflows, coordinate credentialing efforts, and conduct clinical site visits to help you meet internal quality metric goals as well as NCQA requirements.
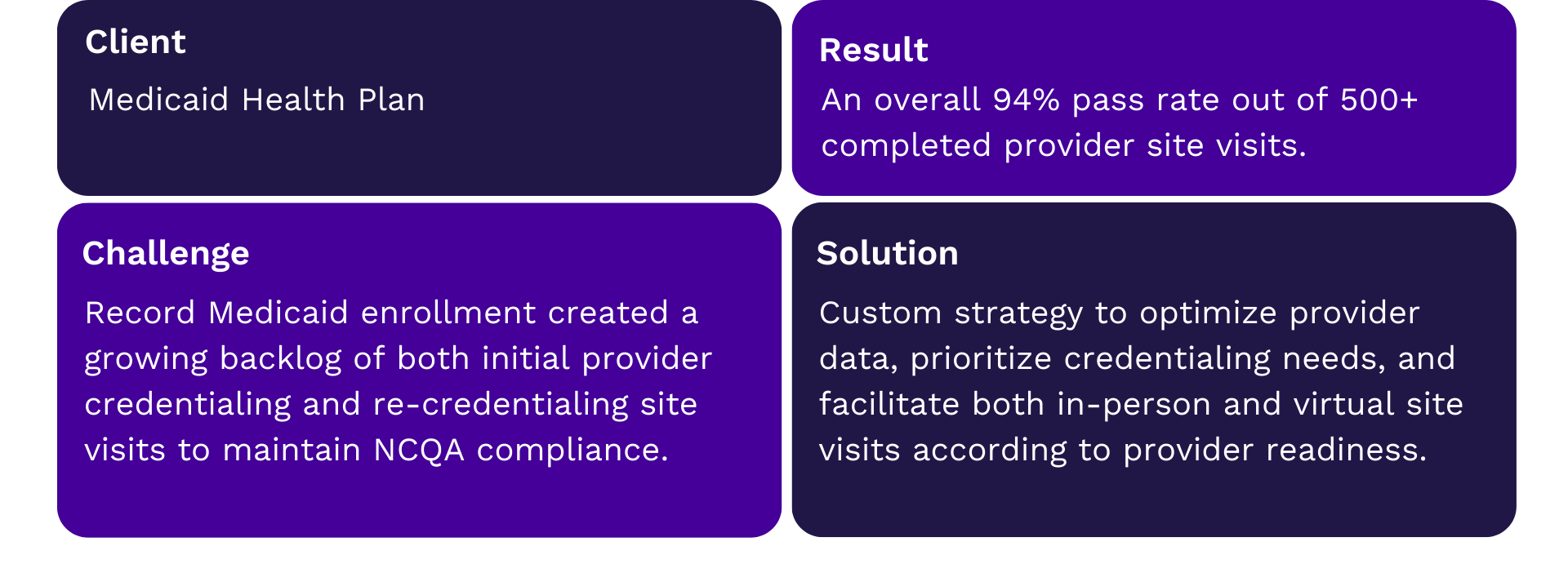
Customer Highlight
We provide expertise, resources, and guidance to address your quality metrics and meet requirements:
Credentialing Experts To Augment Staffing Needs
- Team of registered nurses experienced in conducting Medicaid site visits.
- Corrective action follow-up including evidence-based rationale and partnership with providers to remediate concerns.
- Site visits across a variety of specialties, including mental and behavioral health services, which require the use of specialized criteria to evaluate quality metrics.
Comprehensive Site Visit Management
- Overall planning and coordination by experienced project managers.
- Communication and outreach to provider organizations.
- Site visit execution and follow-up.
- Feedback and provider data updates to health plan.
Flexible Methodology to Accommodate Varying Provider Needs
- HIPAA-compliant in–person and virtual site visits to best meet provider needs.
- Experience working with varying levels of provider technical readiness.
- Schedule and team flexibility to adjust for administrative challenges with provider offices.
We provide:
- Experienced clinical and administrative support staff to augment staffing needs on your existing team or fully outsource site visit facilitation.
- Customized survey tools to meet health plan-specific quality initiatives as well as NCQA required components.
- Collaboration with provider management teams to ensure any updates to provider status, contact information, or other data discovered during site visit facilitation are appropriately recorded and communicated.
We work with:
- Epic, Cerner, Athena, MEDITECH, eClinicalWorks
- Provider management systems such as Symplr, Phind, and Provider Lens
We’ve helped our customers achieve:
- 500+ completed site visits
- Provider outreach within 48 hours
- Availability for site visit within 14 days