Case Study
Improving Patient Access, Physician Experiences at UC Davis Health
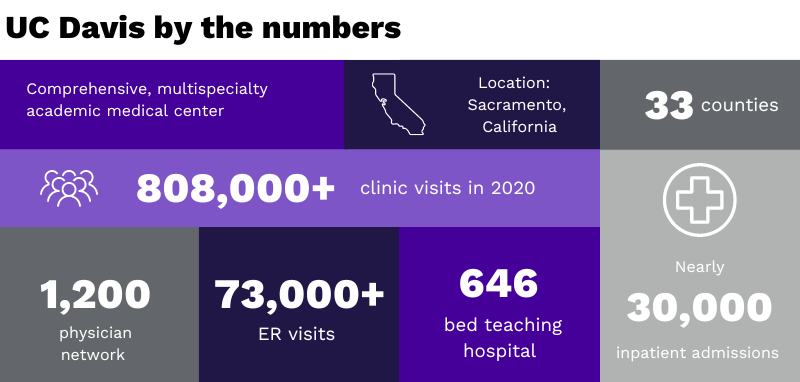
Leading care provider UC Davis Health is optimizing workflows for its people as it reimagines patient contact.
Our healthcare system is complex. And healthcare organizations (HCOs) are becoming larger. Successful HCOs know they need to do more to help patients navigate their own care.
In fact, a recent consumer survey found that half of consumers avoid medical visits because finding, accessing and paying for healthcare is too difficult.1
Some medical providers are working hard to make things easier—and head off potentially serious consequences for people who skip needed care, like worsening health conditions and delayed diagnoses.2 UC Davis Health, a comprehensive medical center in central California, is creating a patient access center (PAC) to simplify everything from appointment scheduling to determining eligibility. Here’s how they are building a centralized service hub that lowers barriers to care.
Start with internal engagement
UC Davis Health’s development of their patient contact center (PCC) has been high touch with hospital leaders, clinicians and medical groups. It’s also been methodical. The PCC planning team visited more than a dozen academic medical centers to observe how other HCOs had centralized their operations. As the team worked to develop a business plan for UC Davis Health’s PCC, they engaged with hospital leadership, as well as affiliated clinics and medical groups, to ensure an enterprise-wide commitment to the initiative.
“Physician engagement and leadership are absolutely critical for planning, problem-solving and support,” said Michael Condrin, Chief Operating Officer, Ambulatory Care at UC Davis Health.
Physicians are a customer of the PCC, also, along with the patients. They need to have a strong voice in making sure a solution meets the needs of the practices and keeps the best interests of the patients at the heart.
MICHAEL CONDRINChief Operating Officer, Ambulatory Care at UC Davis Health
Develop a comprehensive vision
UC Davis Health already had the “nucleus” of centralized operations in place in the form of a Central Access Unit (CAU) that processed internally generated referrals and received external incoming referrals. “The CAU only serviced a portion of our enterprise, not the whole. We knew it was delivering a superior experience for those patient contact points,” explains Condrin.
The PCC planning team’s vision was to expand this centralized approach to improve everyone’s experience—and bring a little more humanity to the patient journey.
Take phone systems, for instance. “Before we began implementing the PCC, we had 40 different phone rooms across our distributed clinics, said Condrin. “As a result, the patient experience was at times inconsistent and volatile. And it wasn’t good for those handling these calls either. We wanted to provide a more standardized, scalable and consistent patient experience.”
Centralized patient contact, from appointments to billing
Most patient access centers offer centralized administrative functions such as appointment scheduling, registration and referral management. UC Davis Health makes the financial aspects of care part of the patient access solution.
It integrates the Financial Clearance Unit (FCU), overseen by the Revenue Cycle team. This equips the PCC to handle tasks like eligibility verification and financial clearance for patients.
Another important feature of UC Davis Health’s PCC implementation is embedded nurse triage. “A big pain point for many patient access centers is clinical escalation on site when calls or referrals require quick clinical review, notes Condrin. “We have an RN team in place that can support the phone staff when, for example, a scheduling event has to be escalated to a clinical emergency event.”
For example, if a patient calls in to make an appointment and mentions that he or she is having trouble breathing, that is beyond the scope of a customer service representative. “With the nurse triage in place, that kind of situation can be escalated and handled in real time,” he said.
Choosing a partner who knows both IT and care
UC Davis Health chose to work with Tegria to bring its vision for a comprehensive PCC to life. “We sought out specialists who had implemented this type of standardized operations at other medical centers. Because we needed broader expertise in this realm than what we had internally. We wanted a company that could help us apply industry best practices and at the same time come up with solutions that were contextual to UC Davis Health’s culture and patient needs,” said Condrin.
Tegria works with organizations to identify, install and optimize the appropriate portfolio of technologies needed to achieve their goals. Because our deep bench of consultants is steeped in both technology and health, we understand what it takes to integrate data, clinical workflows, and organizational strategies.
For UC Davis, we helped with the selection and adoption of an appropriate telephony platform. We also assisted in optimizing the use of the existing EHR (Epic) to support the PCC’s functions.
“It’s important to not just automate existing processes,” notes Condrin. “You need to review and, in many cases, fix underlying workflows before you can automate them. And when you go into an endeavor like this you uncover a whole lot of legacy workflows that you haven’t tackled in years.”
Tegria is helping us identify obstacles in our workflow that don’t align with best practices. We will be better off on a lot of fronts having gone through this transformational process.
MICHAEL CONDRINChief Operating Officer, Ambulatory Care at UC Davis Health
Immediate impact on the patient experience—and ROI
Condrin estimates that UC Davis Health is about a quarter of the way through implementing its complete PCC vision. The medical center is already seeing a return on its investment (ROI). The time taken for scheduling an appointment has dropped by more than 50%. The length of wait time for patients to see providers has shortened by more than seven days.
“Tegria is helping us identify obstacles in our workflow that don’t align with best practices. The critical thinking and the act of fixing broken processes before we automate them in the call center environment is huge value added. We will be better off on a lot of fronts having gone through this transformational process,” Condrin said.